Where most people see overwhelming clutter, Dara Concagh, LICSW, a clinician at Riverside’s Outpatient Center in Newton, sees the person behind the mess. As Riverside’s leading hoarding specialist, Dara doesn’t just help clear physical spaces—she partners with the people she serves to untangle the complex web of emotions, trauma, and psychology that creates these challenging living situations.
In the following article, Dara seeks to reduce stigma and empower growth by answering five common questions about hoarding disorder.
1. What is hoarding disorder?
DC: Hoarding disorder is characterized by an ongoing difficulty to part with your possessions, regardless of their value. Individuals with this condition experience distress when thinking about discarding their belongings and often accumulate more than they need, resulting in living spaces so cluttered they can not be used appropriately.
2. How does hoarding typically develop, and what factors might contribute to its onset?
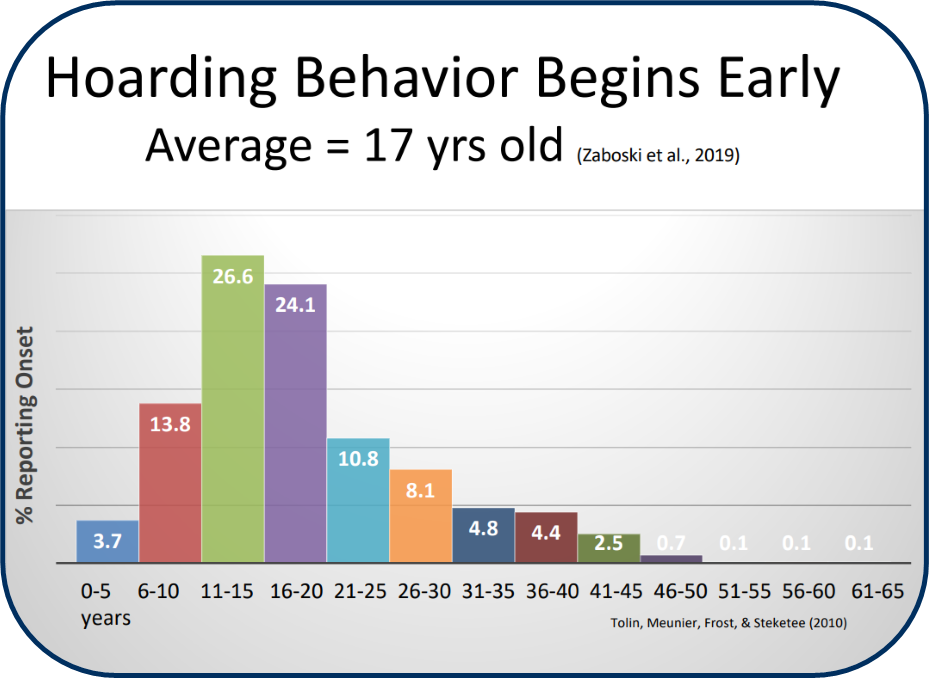
DC: Every individual hoarding case is unique and needs to be recognized as such. However, a popular hoarding disorder model developed by Randy Frost and Gail Steketee (more about them later!) indicates that hoarding behaviors typically develop through a combination of family dynamics and information processing struggles.
Family dynamics can be complicated, and our relationships help shape the world around us. Children growing up in homes where parents hoard often learn that keeping excessive possessions is normal and discarding items is wasteful. Alternatively, individuals with traumatic upbringings may form unhealthy attachments to objects as a substitute for reliable human relationships or accumulate possessions to feel in control amid their unpredictable environments.
Information processing struggles include issues with attention, focus, and perfectionism. Some people avoid throwing out objects due to a fear of making the “wrong” choice, while others just have trouble making decisions in general. These vulnerabilities often interact and reinforce each other, making hoarding a particularly complex condition to address.
3. What is not commonly known about hoarding?
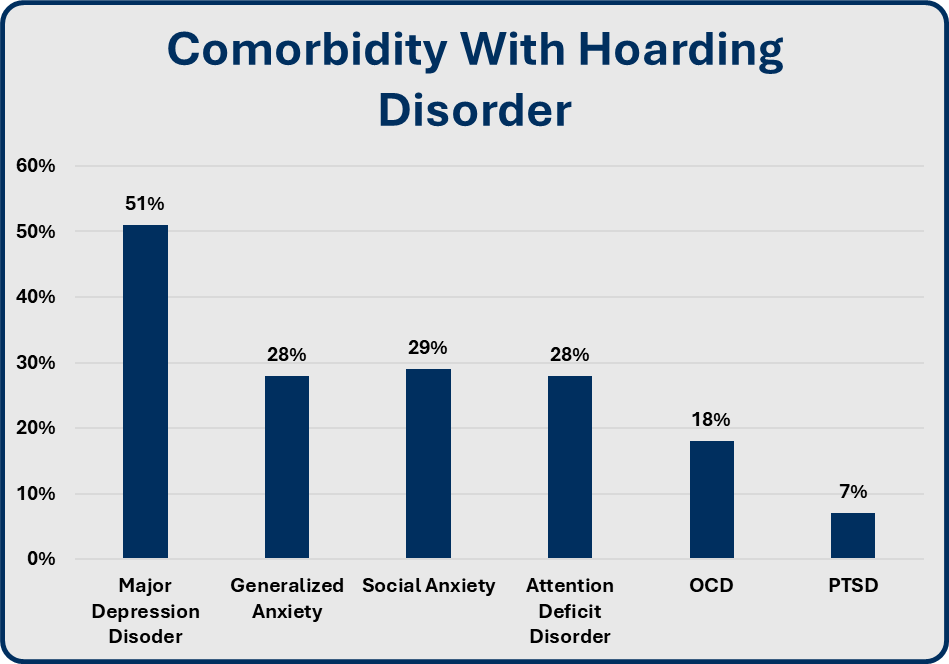
DC: Many people don’t realize that hoarding isn’t always linked to OCD. Originally, mental health professionals thought hoarding symptoms only occurred alongside OCD, and this outdated view persists today. However, people managing hoarding disorder are more likely to have depression as a co-occurring condition.
DC: I also want to make it clear that hoarding disorder isn’t just a case of someone being “lazy” or “messy.” It’s a legitimate mental health condition that needs to be taken seriously. Hoarding leads to significant stress and can put people in danger due to increased fire hazards, blocked exits, and sanitation issues. We need to treat individuals with hoarding disorder with the same level of care and compassion received by anyone managing a physical illness or different psychiatric diagnosis.
4. How can people get help managing hoarding disorder?
DC: At Riverside, we have several groups for people struggling with hoarding. Group therapy is a wonderful modality because it decreases the secrecy and shame that someone with hoarding disorder might feel. Sharing experiences with people who truly understand your situation helps people feel less alone. Additionally, connecting with individuals who have made significant progress in reducing their clutter provides hope and shows that recovery really is possible.
Our groups are guided by the CBT workbook “Treatment for Hoarding Disorder,” written by the previously mentioned clutter experts Gail Steketee and Robert O. Frost. The evidence-based workbook helps individuals understand the thoughts and emotions that lead to hoarding behaviors and develop unique solutions. We also have four ongoing maintenance groups so that clients can remain connected, supported, and accountable after their initial group ends. Additionally, I will run another Introduction to CBT for Hoarding Disorder group with Lori Barry-Smith, LICSW, on Tuesdays at 1 pm via Zoom starting in September. We’re accepting referrals from now through the end of August. Interested clients can contact our intake coordinator, Ty Cribbs, at tcribbs@riversidecc.org or call 781-606-9395.
5. What gives you hope about our ability to better understand and address hoarding in the future?
DC: Through an increase in evidence-based treatment methods including CBT, more and more people can understand the thoughts and emotions that lead to hoarding. Being cognizant of how you feel when acquiring, saving, and holding on to items has been proven to help individuals manage and decrease their clutter. Additionally, the individuals I work with – both colleagues and people served – provide a great deal of hope every day. The people in our hoarding therapy group dedicate themselves to making meaningful changes, and their resilience inspires me.
If you enjoyed this article, be sure to check out the previous addition to our Riverside Insights series: Riverside Insights: 5 Questions for Vic DiGravio About Public Policy Advocacy
